How to use Essential Oils to improve your Microbiome
Most of the time, people think of bacteria as a cause of sickness or disease. But did you know that at all times there are actually billions of beneficial bacteria in our bodies? In fact, bacteria make up our microbiome, an integral internal ecosystem that benefits our gut health and the immune system.
Recently, the scientific community has embraced the important role that bacteria has in fostering a strong immune system and keeping us healthy. Not only are all bacteria not detrimental to our health, but some are actually crucial for boosting immunity, keeping our digestive systems running smoothly, our hormone levels balanced and our brains working properly.
In the modern world, it can be difficult to keep our microbiomes healthy, but there are natural ways to support the ‘good guy’ bacteria in our bodies. Recent research has pointed to essential oils as a way to keep our microbiome in check. We look forward to sharing the fascinating role the microbiome plays in our body, the ways it can be disrupted and the ways it can be supported. But first...
What is the Microbiome?
Trillions of microorganisms make their homes in our bodies. Microbes are involved in almost every single process you can think of, like immune function, nutrient absorption and metabolism- but even things like emotions and decision-making (1). That’s right; microscopic bacteria in your gut can change the way you think and feel. These little guys have such an influence on the brain they can even influence core personality traits, like conscientiousness (2).
However, our microbes maintain a delicate balance which, when disrupted, can wreak havoc on our bodies and minds. Reduced biodiversity and compositional changes in microbiota have been linked to chronic inflammatory diseases like diabetes, obesity, depression, asthma, allergies, multiple sclerosis and Crohn’s disease- and that’s just a sampling of a much longer list.
Risk for many of these diseases are programmed during birth and just afterwards, when our microbiome is first established. A healthy and diverse microbiome teaches our immune system how to work properly. Microbiota crowd out pathogens (bad bacteria and viruses, versus the good microbe kind), helps us absorb nutrients, and even supports us in detoxifying noxious chemicals we might be exposed to on our everyday city commute. An imbalanced microbiome can set us up for a lifetime of inflammation.
But unfortunately, the rates of inflammatory diseases in the modern world are high. You might have heard discussion about the meteoric rise of allergies. It is why most schools won’t allow peanut butter in their cafeterias! The microbiome may actually be the answer to this question. We can reclaim PB&J in our collective diet!
The Rise of Inflammatory Disease in Modern Life
Before urbanization- and long, long before the massive urbanization of the last century- our ancestors ate and lived among microbes, bacteria in the soil, and even human-adapted gut bacteria living as spores in the environment. The commensal microbes developed a relationship with the human immune system. Microbes communicated with, and altered, the function of the immune system, talking to our brains and bodies by mimicking human antigens (your body uses antigens to trigger immune system responses.) In exchange, microbes were allowed to live in our bodies, rent-free.
So what does this have to do with the rise of inflammatory disease? Without normal exposure to microbes like our ancestors had in the soil, for example, our immune systems don’t know how to develop in a healthy way. They overreact to everything. Your Microbiome is like a garden that needs nutrients that we get from nature, and without it, it starts to wilt.
Tip: Take a walk in nature everyday and when you need to rest, sit in the soil and run your fingers through the soil or grass. It might seem unnatural at first, but there could be nothing more natural!
Effects on the body
The pure size of the microbiome is astounding. We have about a 60% - 40% microbe-to-human cell ratio- that means that for every single human cell in your body, there are 1.5 (very non-human) bacterial microbes! (3). But that’s not accounting for all the non-bacterial microbes in our microbiome: trillions of viruses, fungi, and mites, inside and out.
This high number must be maintained. Microbes modulate the immune system, support nutrient absorption, protect against pathogens, maintain barriers to the outside environment, and detoxify foreign substances. But our actions, and even stress levels, can profoundly affect microbial function.
Diet
Even short-term changes in diet can alter microbial composition in the gut. Research reveals significant increases in bacterial gene richness following increased consumption of fruits, vegetables, and dietary fiber. If an intestine is unhealthy, it can become “leaky,” which leads to systemic inflammation and metabolic dysregulation. It is trying to water your garden with a bucket that has a hole. You never get enough nourishment. More frighteningly, impairment of the gut wall not only changes the gut, but can alter immune system function all over the body. The microbiome doesn’t only influence the gut; an unhappy microbiome can influence inflammation at seemingly unrelated sites like the respiratory tract (4).
Our microbes also talk to our brain through neural routes and signaling molecules like neurotransmitters and hormones. This can be affected by diet, too. The microbiome is able to impact “macro” functions like mood and behavior via metabolic activity on dietary components like amino acids. For example, Intestinal microbes are predominantly responsible for the conversion of tryptophan to serotonin (which influences happiness), and change the availability of neurotransmitters that directly and indirectly affect mood (5).
Antibiotics
When it comes to antibiotics, there’s a lot to unpack. Antibiotics have been essential to the successes of modern medicine, but their overuse can create serious and permanent problems. When overused, especially early life, antibiotics exert long-standing effects on the microbiome, including loss of gut microbiota diversity and low-level inflammation. Antibiotic use is associated with an increased risk of obesity, types 1 and 2 diabetes, inflammatory bowel disease, celiac disease, allergies, and asthma (6). We can’t say not to use antibiotics, but caution and moderation are important.
The Impact of Stress on the Microbiome
First of all, psychological stress alters our digestive system, making us more vulnerable to health problems. Stress affects stomach acids and intestine function, which are two mechanisms the gut uses to keep our microbiota in check. Healthy stomach acid prevents colonization of the gut by problematic microbes, while robust intestinal motility sweeps microbes through the digestive tract, out of the small intestine and into the colon where they belong. Impairment of gastric secretions and motility can lead to inflammation and infection.
Environment
We depend on our ecosystems to provide the microbes we need to be healthy. Unfortunately, our modern dwelling spaces aren’t working out so well for our old friends, or for us. Intestinal Dysbiosis (what happens when there is an imbalance in the microbiome) is associated with environmental pollutants (7,8).
Hygiene
Finally, habits of “hygiene” play a key role in our modern anti-microbial mess. But why would keeping myself clean make me sick?, you might ask. Like antibiotics, many products like detergents, hygienic products, soaps, moisturizers, and cosmetics all alter microbial composition, often because they kill both bad bacteria and helpful bacteria. The timing and frequency with which new babies are bathed in the critical developmental window following delivery significantly affects the microbiome. Research suggests that excessive washing with detergents in this period impairs the barrier function of the skin, which increases the risk of eczema (9).
Essential Oils
Some essential oils have been found to affect the microbiome, inhibiting the growth of potential pathogens (the bad guys/weeds) while promoting populations of beneficial commensals (the good guys, AKA our microbes AKA flowers.)
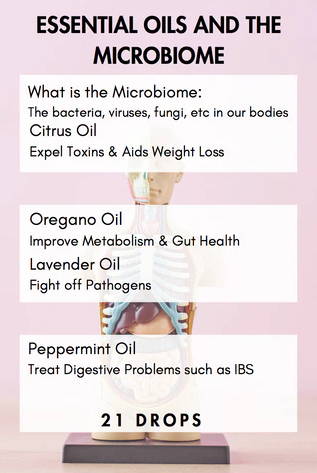
A 2018 study published in Biochemical and Biophysical Research Communications found that orally-administered orange (Citrus ×sinensis) essential oil altered the gut bacteria of obese rats. Sweet orange essential oil protected the gut barrier by increasing the prevalence of friendly bacteria, which reduced toxins and inflammation, and resulted in weight loss in obese rats (10).
Another 2018 study published in Frontiers in Microbiology found that essential oil constituents carvacrol and thymol (most often found in oregano essential oil) modified the intestinal microbial composition and metabolism in weaned piglets in similar ways. Microbial changes were characterized by an increase in the relative abundances of beneficial bacterial species, and a decrease in potential pathogens.
A 2012 study published in the American Journal of Physiology found that lavender essential oil performed similarly well in mice, resulting in less severe disease (11).
Similar findings have been reported in in vitro studies of the human gut microbiome; in vitro refers to using real human cells, but outside the human body (in a petri dish.) It has been found that essential oils like lavender inhibit the growth of potential pathogens while leaving commensals unaffected (12).
A particularly well-researched topic is the use of peppermint oil to treat irritable bowel syndrome (IBS) and its primary trigger, small intestinal bacterial overgrowth (SIBO). SIBO — the inappropriate expansion of colon bacteria into the small intestine — is often caused by intestinal stasis (impaired intestinal motility) and/ or hypochlorhydria (clinically low stomach acid). This can be caused by factors like stress, medication, and diet.
A 2019 meta-analysis of 12 studies with 835 patients published in BioMed Central Complementary and Alternative Medicine likewise reports that peppermint oil is “a safe and effective therapy for pain and global symptoms in adults with IBS.”
In conclusion, the research into essential oils and the microbiome is young but promising, and will most likely continue to expand in the coming years. For now, give your friendly bacteria a pat on the back (in spirit), stay healthy, be careful about those antibiotics, and use your essential oils!
- Prescott, S. L., Wegienka, G., Logan, A. C., & Katz, D. L. (2018). Dysbiotic drift and biopsychosocial medicine: how the microbiome links personal, public and planetary health. Biopsychosocial Medicine, 12. https://doi.org/10.1186/s13030-018-0126-z
- Kim, H.-N., Yun, Y., Ryu, S., Chang, Y., Kwon, M.-J., Cho, J., … Kim, H.-L. (2018). Correlation between gut microbiota and personality in adults: A cross-sectional study. Brain, Behavior, and Immunity, 69, 374–385. https://doi.org/10.1016/j.bbi.2017.12.012
- Zhu, B., Wang, X., & Li, L. (2010). Human gut microbiome: the second genome of the human body. Protein & Cell, 1(8), 718–725. https://doi.org/10.1007/s13238-010-0093-z
- Prescott, S. L., Wegienka, G., Logan, A. C., & Katz, D. L. (2018). Dysbiotic drift and biopsychosocial medicine: how the microbiome links personal, public and planetary health. Biopsychosocial Medicine, 12. https://doi.org/10.1186/s13030-018-0126-z
- van de Guchte, M., Blottière, H. M., & Doré, J. (2018). Humans as holobionts: implications for prevention and therapy. Microbiome, 6(1), 81. https://doi.org/10.1186/s40168-018-0466-8
- Prescott, S. L., Millstein, R. A., Katzman, M. A., & Logan, A. C. (2016). Biodiversity, the human microbiome and mental health: moving toward a new clinical ecology for the 21st century? International Journal of Biodiversity, 2016, 1–18. https://doi.org/10.1155/2016/2718275
- Prescott, S. L., Wegienka, G., Logan, A. C., & Katz, D. L. (2018). Dysbiotic drift and biopsychosocial medicine: how the microbiome links personal, public and planetary health. Biopsychosocial Medicine, 12. https://doi.org/10.1186/s13030-018-0126-z
- Dowd, J. B., & Renson, A. (2018). “Under the skin” and into the gut: social epidemiology of the microbiome. Current Epidemiology Reports, 5(4), 432–441. https://doi.org/10.1007/s40471-018-0167-7
- Li, D., Wu, H., Dou, H., Guo, L., & Huang, W. (2018). Microcapsule of sweet orange essential oil changes gut microbiota in diet-induced obese rats. Biochemical and Biophysical Research Communications, 505(4), 991–995. https://doi.org/10.1016/j.bbrc.2018.10.035
- Li, Y., Fu, X., Ma, X., Geng, S., Jiang, X., Huang, Q., … Han, X. (2018). Intestinal microbiome-metabolome responses to essential oils in piglets. Frontiers in Microbiology, 9. https://doi.org/10.3389/fmicb.2018.01988
- Thapa, D., Louis, P., Losa, R., Zweifel, B., & Wallace, R. J. (2015). Essential oils have different effects on human pathogenic and commensal bacteria in mixed faecal fermentations compared with pure cultures. Microbiology (Reading, England), 161(Pt 2), 441–449. https://doi.org/10.1099/mic.0.000009
- Logan, A. C., & Beaulne, T. M. (2002). The treatment of small intestinal bacterial overgrowth with enteric-coated peppermint oil: a case report. Alternative Medicine Review: A Journal of Clinical Therapeutic, 7(5), 410–417.
About the Author: Kavita Sahai, The Founder
Kavita Sahai has worked in the wellness industry for over a decade and is a certified expert in aromatherapy, Ayurveda, yoga, and nutrition, with a rich background in human design and beauty oils. Kavita combines traditional wisdom with modern research to offer holistic wellness and beauty insights. Focused on sustainable self-care practices, Kavita guides individuals towards achieving both internal and external radiance. She hold an undergraduate degree from the University of Florida and a Master's from UC Berkeley.





